Borderline ECG readings often leave healthcare professionals and patients alike questioning the implications of such results. The term "borderline" in ECG results refers to findings that are not definitively normal or abnormal, but instead fall within a gray area. Understanding the meaning behind borderline ECG results is crucial for anyone who has undergone an electrocardiogram (ECG) and received such an outcome.
ECG tests play a pivotal role in diagnosing heart conditions and monitoring heart health. However, when the results come back as borderline, it can lead to confusion and uncertainty. This article aims to clarify what borderline ECG means, its implications, and what steps individuals should take upon receiving such a diagnosis.
By the end of this guide, readers will have a clearer understanding of borderline ECG findings and how to approach them. Whether you're a healthcare professional, a patient, or someone interested in cardiovascular health, this article provides valuable insights into interpreting and managing borderline ECG results.
Read also:Robin Leach Partner An Indepth Look At The Iconic Celebritys Life And Collaborations
Table of Contents:
- What is Borderline ECG?
- How Does an ECG Work?
- Common ECG Findings
- Causes of Borderline ECG Results
- Challenges in Interpreting Borderline ECGs
- Importance of Follow-Up
- Lifestyle Changes for Heart Health
- Medical Interventions for Borderline ECG
- Preventive Measures for Heart Health
- Conclusion and Next Steps
What is Borderline ECG?
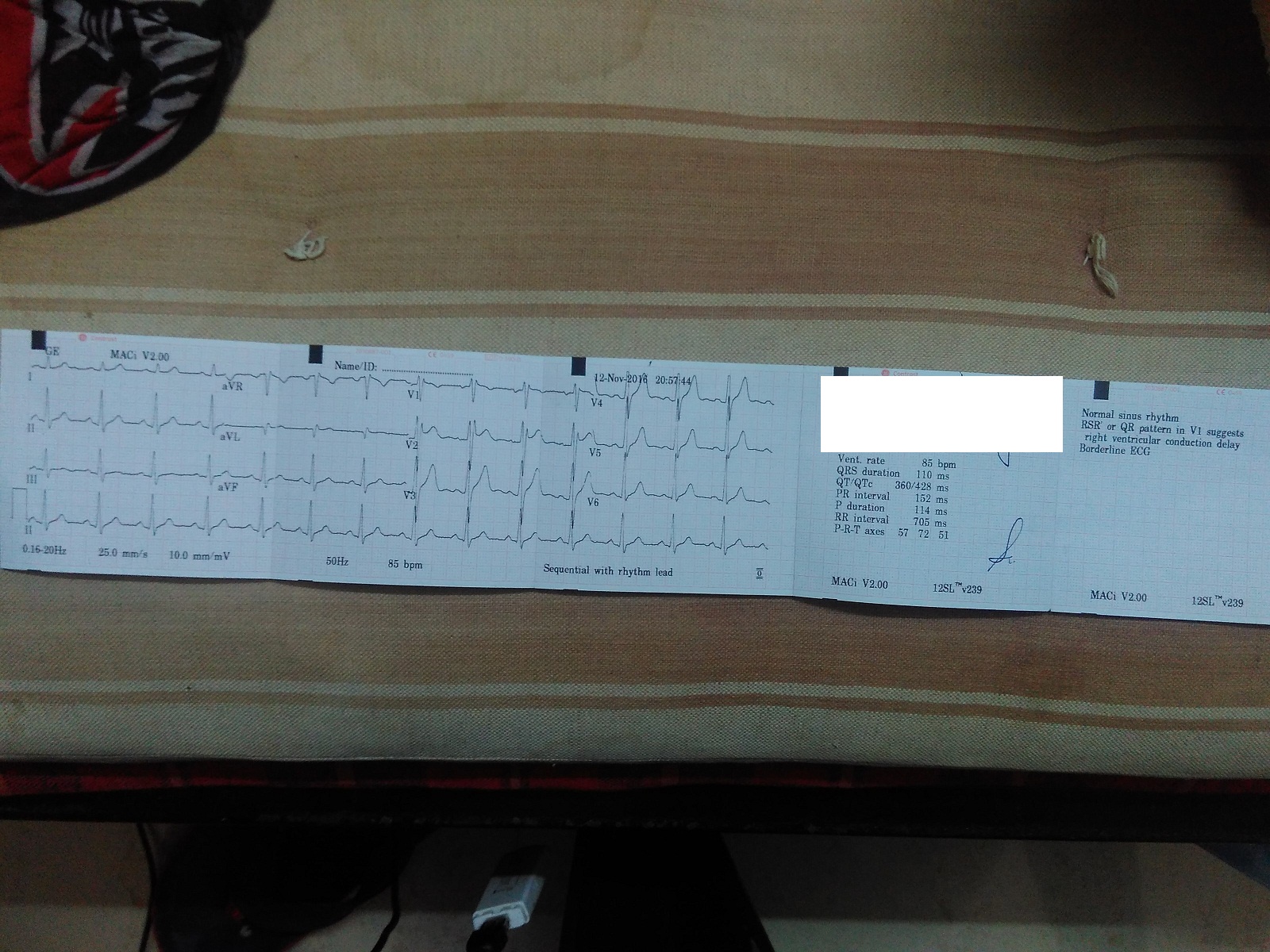
An electrocardiogram (ECG) is a diagnostic tool used to measure the electrical activity of the heart. When the results of an ECG are labeled as "borderline," it signifies that the findings are neither entirely normal nor definitively abnormal. This can include minor deviations in heart rhythm, slight irregularities in intervals, or subtle changes in waveforms that do not meet the criteria for a clear diagnosis.
The term "borderline" in ECG results often arises due to variations in individual physiology. Some people naturally have ECG patterns that differ slightly from the standard norm, but these variations do not necessarily indicate a pathological condition. Understanding the context and clinical significance of borderline ECG findings is essential for accurate interpretation.
Importance of Context in Borderline ECG
When interpreting borderline ECG results, it is crucial to consider the patient's clinical history, symptoms, and overall health. For example, a borderline finding in a young, asymptomatic individual may carry less significance than the same finding in an older person with a history of heart disease. Contextual analysis ensures that borderline ECG results are not overinterpreted or overlooked.
How Does an ECG Work?
An ECG works by detecting and recording the electrical signals that control heartbeats. These signals are captured through electrodes placed on the skin and translated into a graph that displays the heart's rhythm and electrical activity. The ECG graph consists of waves, intervals, and segments that correspond to different phases of the cardiac cycle.
Understanding how an ECG works helps in appreciating the nuances of borderline ECG findings. Minor variations in these waves and intervals can sometimes be misinterpreted as abnormal, especially if the clinician lacks familiarity with the patient's baseline ECG patterns.
Read also:Jon Voight The Iconic Journey Of A Legendary Actor
Types of ECG Tests
- Resting ECG: Performed while the patient is at rest.
- Exercise ECG (Stress Test): Conducted during physical activity to assess heart performance under stress.
- Holter Monitor: A portable device worn for 24-48 hours to record continuous ECG data.
Common ECG Findings
ECG results can range from normal to abnormal, with borderline findings occupying the intermediate space. Common ECG findings include:
- Normal sinus rhythm: Indicates a regular heartbeat originating from the sinus node.
- Bradycardia: A slower-than-normal heart rate.
- Tachycardia: A faster-than-normal heart rate.
- Atrial fibrillation: An irregular and often rapid heart rhythm.
Borderline ECG findings may involve slight deviations from these patterns, such as mildly prolonged QT intervals or minor ST-segment changes.
Interpreting ECG Results
Interpreting ECG results requires a thorough understanding of the heart's electrical activity. Clinicians must consider factors such as age, gender, and underlying medical conditions when evaluating borderline ECG findings. For instance, athletes often exhibit ECG patterns that differ from the general population due to their cardiovascular adaptations.
Causes of Borderline ECG Results
Several factors can contribute to borderline ECG findings, including:
- Physiological Variations: Normal differences in heart anatomy and function.
- Medications: Certain drugs can alter ECG patterns.
- Electrode Placement: Improper placement of electrodes may lead to inaccurate readings.
- Underlying Conditions: Subclinical heart conditions may manifest as borderline ECG findings.
Identifying the underlying cause of borderline ECG results is essential for appropriate management and follow-up.
Role of Medications in ECG Changes
Some medications, such as beta-blockers, antiarrhythmics, and electrolyte-altering drugs, can influence ECG patterns. Clinicians must account for these effects when interpreting borderline ECG findings and adjust treatment plans accordingly.
Challenges in Interpreting Borderline ECGs
Interpreting borderline ECGs poses several challenges, including:
- Variability in Standards: Different institutions may use slightly different criteria for normal and abnormal ECG findings.
- Clinical Context: Lack of comprehensive patient history can hinder accurate interpretation.
- Subjectivity: Interpretation of borderline ECGs can be subjective, depending on the clinician's experience and expertise.
Addressing these challenges requires a multidisciplinary approach, involving collaboration between cardiologists, electrophysiologists, and other healthcare professionals.
Technological Advancements in ECG Analysis
Recent advancements in artificial intelligence and machine learning have improved the accuracy of ECG interpretation. These technologies can assist clinicians in identifying subtle patterns and nuances that may be missed during manual analysis.
Importance of Follow-Up
Follow-up is critical for individuals with borderline ECG findings. Regular monitoring and repeat testing can help determine whether the findings are transient or indicative of an underlying condition. Follow-up may involve:
- Repeat ECG testing.
- Additional diagnostic tests, such as echocardiography or stress testing.
- Referral to a cardiologist for further evaluation.
Proactive follow-up ensures that any potential issues are identified and addressed promptly, minimizing the risk of complications.
Lifestyle Changes for Heart Health
Adopting a heart-healthy lifestyle can help mitigate the risks associated with borderline ECG findings. Key lifestyle modifications include:
- Maintaining a balanced diet rich in fruits, vegetables, and whole grains.
- Engaging in regular physical activity.
- Avoiding smoking and excessive alcohol consumption.
- Managing stress through relaxation techniques and mindfulness practices.
Medical Interventions for Borderline ECG
In some cases, medical interventions may be necessary to address borderline ECG findings. These interventions may include:
- Medication adjustments to correct electrolyte imbalances or manage arrhythmias.
- Implantable devices, such as pacemakers or defibrillators, for severe cases.
- Interventional procedures, such as catheter ablation, for refractory arrhythmias.
Medical interventions should always be guided by a thorough evaluation of the patient's clinical status and ECG findings.
Preventive Measures for Heart Health
Preventive measures play a vital role in maintaining heart health and preventing borderline ECG findings from progressing to more serious conditions. Strategies for prevention include:
- Regular health check-ups and screenings.
- Monitoring and managing risk factors such as hypertension, diabetes, and high cholesterol.
- Staying informed about cardiovascular health through education and awareness programs.
Conclusion and Next Steps
Borderline ECG findings represent a gray area in cardiac diagnostics, requiring careful interpretation and management. By understanding the meaning of borderline ECG results and taking appropriate steps, individuals can safeguard their heart health and minimize the risk of complications.
We encourage readers to:
- Discuss borderline ECG findings with their healthcare provider for personalized advice.
- Adopt heart-healthy lifestyle changes to support cardiovascular well-being.
- Stay informed about advancements in ECG technology and heart health management.
Share this article with others who may benefit from its insights and explore additional resources on our website for further information on heart health and ECG interpretation.
References:
- American Heart Association. (2022). Understanding ECG Results. Retrieved from [AHA Website].
- Mayo Clinic. (2021). Electrocardiogram (ECG or EKG). Retrieved from [Mayo Clinic Website].
- World Health Organization. (2023). Cardiovascular Health Guidelines. Retrieved from [WHO Website].